It’s been a whirlwind decade for reproductive health.
The country has simultaneously witnessed women’s access to health services expanded, through cancer-preventing vaccines and no-cost contraception, as well as limited by the unprecedented rise in abortion restrictions in states nationwide.
Although she’s concerned about the abortion battles still playing out in the courts, Dr. Katie McHugh, an OB-GYN in Indiana and junior fellow leader at the American College of Obstetricians and Gynecologists, says she’s also hopeful about what’s to come.
“I’m an optimist,” McHugh said. “Having the chance to look back and see successes and failures is nothing less than an opportunity to do better for the next decade.”
As we shift decades, here are five key moments in reproductive health over the past 10 years:
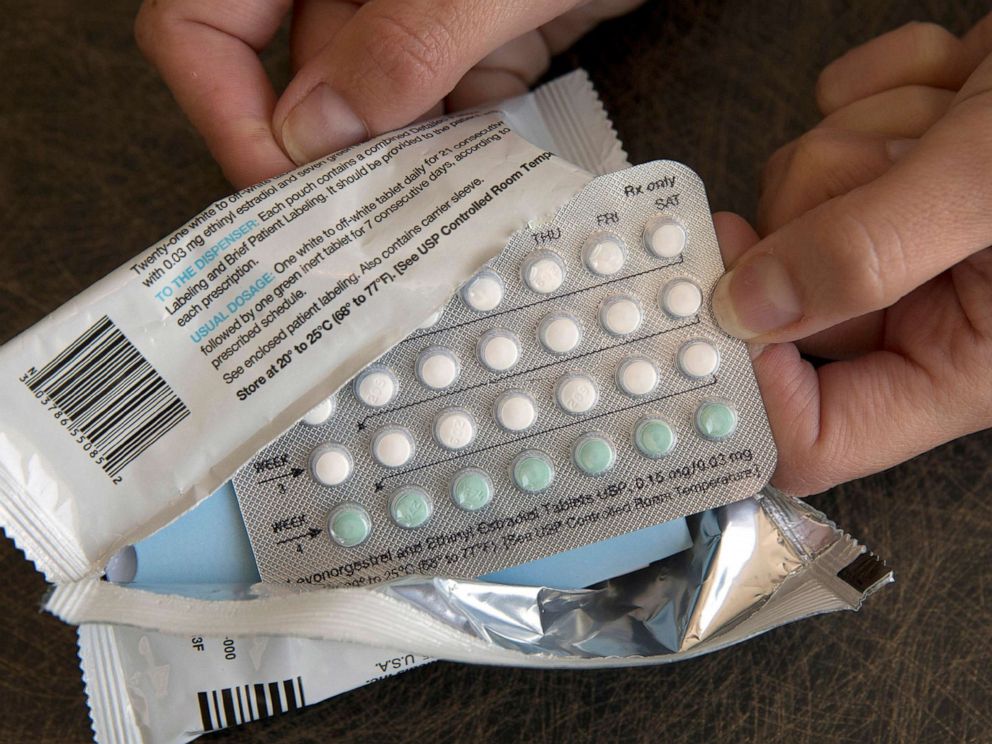
1. The Affordable Care Act transforms birth control coverage
 Rich Pedroncelli/AP, FILE
Rich Pedroncelli/AP, FILE
When the Affordable Care Act was enacted in 2010, it included an important mandate for women’s health: private health insurance plans were required to cover contraception costs.
In short, millions of American women now had access to birth control, without having to pay out of pocket for it.
For some women, this lessened the financial burden they were shouldering to pay for the birth control pill, saving them $255 per year on average. For others, the additional coverage allowed them to access more reliable, but formerly more expensive, forms of birth control.
Increased access led to real-world behavior shifts. Women’s out-of-pocket birth control expenses fell. There was also a small, but significantly significant increase in women getting long-acting reversible contraception, like the IUD, according to a study published in the journal Women’s Health Issues.
“It was this twofer,” Elizabeth Nash, senior state issues manager in the Guttmacher Institute, said of the ACA. “With millions more covered, and much better coverage, it really improved access to contraception.”
2. Republican election wins trigger a wave of state-level abortion restrictions
 AFP via Getty Images, FILE
AFP via Getty Images, FILE
Following the 2010 elections, when a slew of Republican and Tea Party candidates swept into state office, abortion restrictions started being passed en masse.
“In January 2011, you started to see abortion restrictions flying through the state legislatures,” Nash said.
Since then, 33 states, primarily in the South, Midwest and Plains regions, have enacted 483 restrictions ranging from mandated counseling and waiting periods before an abortion to consent notification for minors to limits on public funding for abortion.
More abortion restrictions were enacted between 2010 and 2015 than during any other five-year period since Roe v. Wade, according to the Guttmacher Institute, a nonprofit research and policy organization that studies and advocates for sexual and reproductive rights.
Restrictions in Indiana have made it difficult for McHugh, an abortion provider, to do her job.
One state restriction, which requires patients to visit a facility twice in order to receive an abortion, creates a barrier for McHugh’s patients who live long distances from the clinic. McHugh says it’s not uncommon for those patients to be unable to attend the second visit, which is when the abortion is actually performed.
The end result: Women delivering babies they didn’t plan on having, she says.
“This is a change in the last 10 years that has made health care more dangerous, made health care worse for people and changed the course of people’s lives in a real way,” McHugh said.
“It’s really hard for me to see how a movement like that has a patients’ best interests in mind.”
3. Whole Woman’s Health Supreme Court decision halts abortion restrictions
 Sipa via AP, FILE
Sipa via AP, FILE
In 2016, the Supreme Court struck down abortion restrictions in Texas and reaffirmed the constitutional right to abortion access that Roe v. Wade established in the landmark case, Whole Woman’s Health v. Hellerstedt.
Those restrictions — including requiring physicians to have admitting privileges at a nearby hospital and abortion clinics to maintain conditions comparable to ambulatory surgical centers — placed an “undue burden” on women’s ability to receive abortions, the court ruled.
“It was a turning point in abortion legislation,” McHugh said, noting that since those restrictions weren’t based in science, they primarily made health care more expensive and harder to get for women.
Despite the back-and-forth over abortion restrictions over the past decade, Whole Women’s Health set an important precedent by effectively slowing the progress of abortion restrictions in states across the country.
However, the push-and-pull continues, with the Supreme Court slated to hear a similar case out of Louisiana, which notably will be heard by different justices, including the more conservative Brett Kavanaugh, potentially resulting in a different outcome.
4. The HPV vaccine scales up to include middle-age adults — and men
 Boston Globe via Getty Images, FILE
Boston Globe via Getty Images, FILE
While the Food and Drug Administration approved the HPV vaccine for girls and women between the ages of 9 and 26 in 2006, the last 10 years saw that approval expand to include people as old as 45 — as well as boys and men.
Since human papillomavirus causes nearly all cervical cancers, according to the Centers for Disease Control and Prevention, and is linked to various other types of cancer, preventing the cancer-causing sexually transmitted disease, which 79 million American are infected with, is a high priority for reproductive health experts.
“Vaccines are revolutionary in their ability to change the course of a disease in a population,” McHugh said.
“The fact that it can prevent cancer in people is nothing short of a science miracle.”
5. U.S. starts taking maternal mortality seriously
 Seth Wenig/AP, FILE
Seth Wenig/AP, FILE
While global maternal mortality has been falling in recent decades, in the United States, the number of women dying in childbirth has been rising. There’s also a racial disparity at play. African-American women are three to four times more likely to die during childbirth as white women are, according to the CDC.
“It is a really, really scary time to be pregnant in the United States,” McHugh said. “In the last 10 years, the trend has become so pronounced that it’s impossible to ignore.”
For the public, a touchstone moment came in 2018, when professional tennis player Serena Williams revealed that she’d nearly died of pregnancy-related complications in the days following the birth of her daughter Olympia.
Whether it’s the statistics, high-profile stories like Williams’, or both, lawmakers are finally taking the maternal mortality seriously.
Last December, Congress passed legislation to fund collecting and analyzing data on maternal deaths across the United States.
And this year,
Democratic candidates for president, including Sens. Elizabeth Warren and Kamala Harris, have made maternal mortality — and their plans to prevent maternal deaths in the United States — a talking point on the campaign trail.


