As officials scramble to supply hospitals with much needed protective equipment for doctors and nurses fighting the novel coronavirus on the front lines, hospital leaders around the country warn that they are running low on another critical supply: money.
Hospitals have taken a significant loss of revenue as they cut back lucrative elective procedures to free up resources to treat COVID-19 patients. At the same time, they are pouring money into efforts to fight the virus like buying personal protective equipment (PPE) supplies, providing child care for staff and overtime pay, transforming units to COVID-19 wings for treatment and setting up drive-thru testing sites, hospital officials told ABC News.
New York Gov. Andrew Cuomo this week called the combination a “double whammy.” For hospital systems across the country the costs are astronomical and state officials told ABC News they fear some facilities do not have enough cash to keep up.
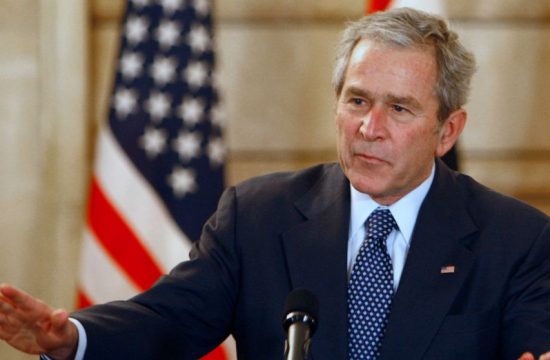
The $2 trillion stimulus package President Donald Trump signed on Friday afternoon, which awards nearly $100 billion to hospitals to fight the coronavirus, is a boost many hope will alleviate some of the financial burden and prevent hospitals from closing their doors.
“We can’t print money, so we have to have the financial support coming in.” LeRay Brown, the CEO of One Brooklyn Health System, told ABC News. “Without that funding I don’t know how long we can continue.”
One Brooklyn Health System, which operates three hospitals in New York City where the virus has hit hardest in the U.S., projects they will need to spend an additional $30 million per month in order to respond to surge needs in their area, Brown said, including the nearly $8 million they will lose per month by cutting out elective surgeries. Purchasing nearly 300 additional beds in order to increase hospital’s capacity by 50% — which they have been mandated to do under an executive order signed by Cuomo — will cost $5 million alone.
The hospital system, which is crucial for low-income individuals in the area, is already caring for over 200 patients who either have the virus or are awaiting test results. Meanwhile, it only has two weeks cash on hand, Brown said.
One doctor on the front lines said they feel hospitals are being overlooked in the national dialogue about the extreme toll the pandemic has taken on the U.S. economy.
“I think there’s been so much national focus on bailing out the airlines, but I think what people don’t realize is that the hospitals are in extreme financial trouble over the COVID-19 crisis,” a physician at a top Boston area hospital told ABC News. “I feel like people — nobody’s talking about that. Everybody thinks hospitals are doing fine. If we don’t bail out the hospitals, we’re going to lose the very lifelines that we have — the front lines that we have — to fight this thing.”
What to know about coronavirus:
During the signing of the stimulus bill, Trump did acknowledge the challenge hospitals are facing, saying more than $100 billion is going to “support our heroic doctors, nurses and hospitals” and that hospitals will get “the money they need.”
American Hospital Association President and CEO Rick Pollack called the legislation an “important first step forward,” but warned that “more will need to be done to deal with the unprecedented challenge of this virus.”
Hospital leaders in numerous states echoed the dire concerns about their facilities and the urgent need for an infusion of funding.
Andy Carter, the president and CEO of the Hospital and Healthsystem Association of Pennsylvania (HAP), said there is a “legitimate credible threat” that some hospitals in his state would close without immediate financial support.
An HAP spokesperson told ABC News the federal package was “encouraging,” but warned there was no “clarity” on how much aid would be distributed to hospitals in the state — or when.
“We caution that some of our members have estimated, and nationwide accounts validate, that hospitals are facing a financial free-fall,” the spokesperson wrote, explaining that a “preliminary analysis” shows that losses for hospitals in Pennsylvania alone could rise to more than $1 billion per month.
In Ohio, President of the Ohio Hospital Association Mike Abrams said he could think of two hospitals that he “worries a lot about,” and could “think of many more” that will be in equally precarious situations if aid does not come soon. The TriHealth system, based in Cincinnati, has already cut 20% of senior leader’s pay in order “be fully prepared for the surge in demand,” Chief Executive Officer Mark Clement said in a statement, as reported by Cincinnati.com.
Jeff Tieman, president and CEO of the Vermont Association of Hospitals and Health Systems, explained the increase in costs are especially significant for rural hospitals that were already “under serious financial stress” even before the pandemic began in the state of Vermont, which has one of the oldest populations in the country,
Minnesota-based health system M Health Fairview, which recently converted one of its hospitals to a COVID-19 specialized-care facility, is anticipating a cut of more than a third of its revenue due to loss of volume in outpatient areas, spokesperson David Henke told ABC News. As a nonprofit group that operates on a extremely tight margins — with net operating margin for last fiscal year at just 0.2% — Fairview faces significant financial challenges as a result of the pandemic, Henke said.
“Our focus right now is providing the care our patients and our community need,” Henke told ABC News. “However, the reality is M Health Fairview, like many health care systems across the country, is facing unprecedented challenges as a result of this public health crisis.”
And the financial crunch is a reality hospitals across the financial spectrum are dealing with.
“Even the hospitals who are well resourced are really worried,” Abrams told ABC News. He estimates the fiscal impact on Ohio hospitals would amount to a loss of $1.2 billion per month. “It is effecting everyone negatively, whether you are a huge system that is well resourced or a small system that was hanging on nervously.”
The Hospital for Special Surgery in New York said the cost of scaling back their capacity by 90% in order to brace for a surge and transforming their facilities, coupled with the loss in revenue, amounted to “hundreds of million of dollars,” CEO Lou Shapiro told ABC News.
In Louisiana, where the number of positive cases and deaths is skyrocketing, Baton Rouge General Hospital has also backed away from its outpatient business as it doubles down on its COVID-19 response while continuing to provide essential care for those having heart attacks, strokes, diabetes or cancer.
Completely letting go of the highly lucrative elective surgery has caused a big financial strain on the system, its CEO Stephen Mumford told ABC News. Mumford said on Thursday there were less than five surgeries, all of which were emergent surgeries.
“When you go from a hospital that does 40 to 50 surgeries a day to a hospital that does two to three, it really is going to hurt us,” Mumford said.
“But the reality is, we can’t worry about that right now,” Mumford said. “We’re a community hospital and we’ve got to take care of the community patients that are coming in.”
Tune into ABC at 1 p.m. ET and ABC News Live at 4 p.m. ET every weekday for special coverage of the novel coronavirus with the full ABC News team, including the latest news, context and analysis.
ABC News’ Ali Dukakis contributed to this report.